Understanding Fainting: Causes, Symptoms, and Management
Related Articles: Understanding Fainting: Causes, Symptoms, and Management
Introduction
In this auspicious occasion, we are delighted to delve into the intriguing topic related to Understanding Fainting: Causes, Symptoms, and Management. Let’s weave interesting information and offer fresh perspectives to the readers.
Table of Content
Understanding Fainting: Causes, Symptoms, and Management
:max_bytes(150000):strip_icc()/1298399-article-img-causes-of-fainting1-5a5520127bb283003773f0c9.png)
Fainting, also known as syncope, is a sudden, brief loss of consciousness caused by a temporary decrease in blood flow to the brain. This decrease in blood flow can result from various factors, ranging from simple physiological responses to underlying medical conditions. While fainting can be alarming, it is often harmless and resolves on its own. However, understanding the underlying causes is crucial for determining the appropriate management strategy and preventing future episodes.
Causes of Fainting
The causes of fainting can be broadly categorized into three main groups:
1. Neurocardiogenic Syncope (Vasovagal Syncope):
This is the most common type of fainting, accounting for approximately 50% of cases. It is triggered by a sudden drop in blood pressure and heart rate, often due to a combination of factors:
- Emotional Stress: Fear, anxiety, pain, or emotional distress can trigger the vagus nerve, which controls heart rate and blood pressure, causing a sudden decrease in both.
- Pain: Sharp, sudden pain, such as from a needle stick or a cut, can also activate the vagus nerve, leading to fainting.
- Stressful Situations: Situations like standing for prolonged periods, dehydration, or exposure to heat can also contribute to vasovagal syncope.
- Blood Donation: The process of blood donation can sometimes lead to vasovagal syncope due to the sudden loss of blood volume.
- Gastrointestinal Issues: Nausea, vomiting, or bowel movements can also trigger vasovagal syncope.
2. Situational Syncope:
This type of fainting is associated with specific situations or activities that trigger a decrease in blood flow to the brain:
- Orthostatic Hypotension: This occurs when there is a sudden drop in blood pressure upon standing up, often due to dehydration, medication side effects, or certain medical conditions.
- Carotid Sinus Syncope: This is caused by pressure on the carotid artery in the neck, which can be triggered by tight collars, turning the head quickly, or shaving.
- Cough Syncope: This occurs during prolonged or forceful coughing, which can increase pressure in the chest cavity, reducing blood flow to the brain.
- Micturition Syncope: This type of fainting occurs during or immediately after urination, particularly in elderly individuals.
- Postural Syncope: This refers to fainting that occurs after prolonged standing or sitting, especially in hot environments.
3. Cardiac Syncope:
This type of fainting is caused by problems with the heart, which can disrupt the flow of blood to the brain:
- Arrhythmias: Irregular heart rhythms, such as bradycardia (slow heart rate) or tachycardia (fast heart rate), can lead to fainting.
- Heart Valve Disease: Fainting can occur due to the inability of the heart valves to function properly, leading to reduced blood flow.
- Congenital Heart Disease: Some individuals with congenital heart defects may experience fainting due to impaired heart function.
- Coronary Artery Disease: Blockage of the coronary arteries, which supply blood to the heart, can lead to heart attack and fainting.
- Pulmonary Embolism: A blood clot in the lungs can cause a sudden decrease in oxygen levels, leading to fainting.
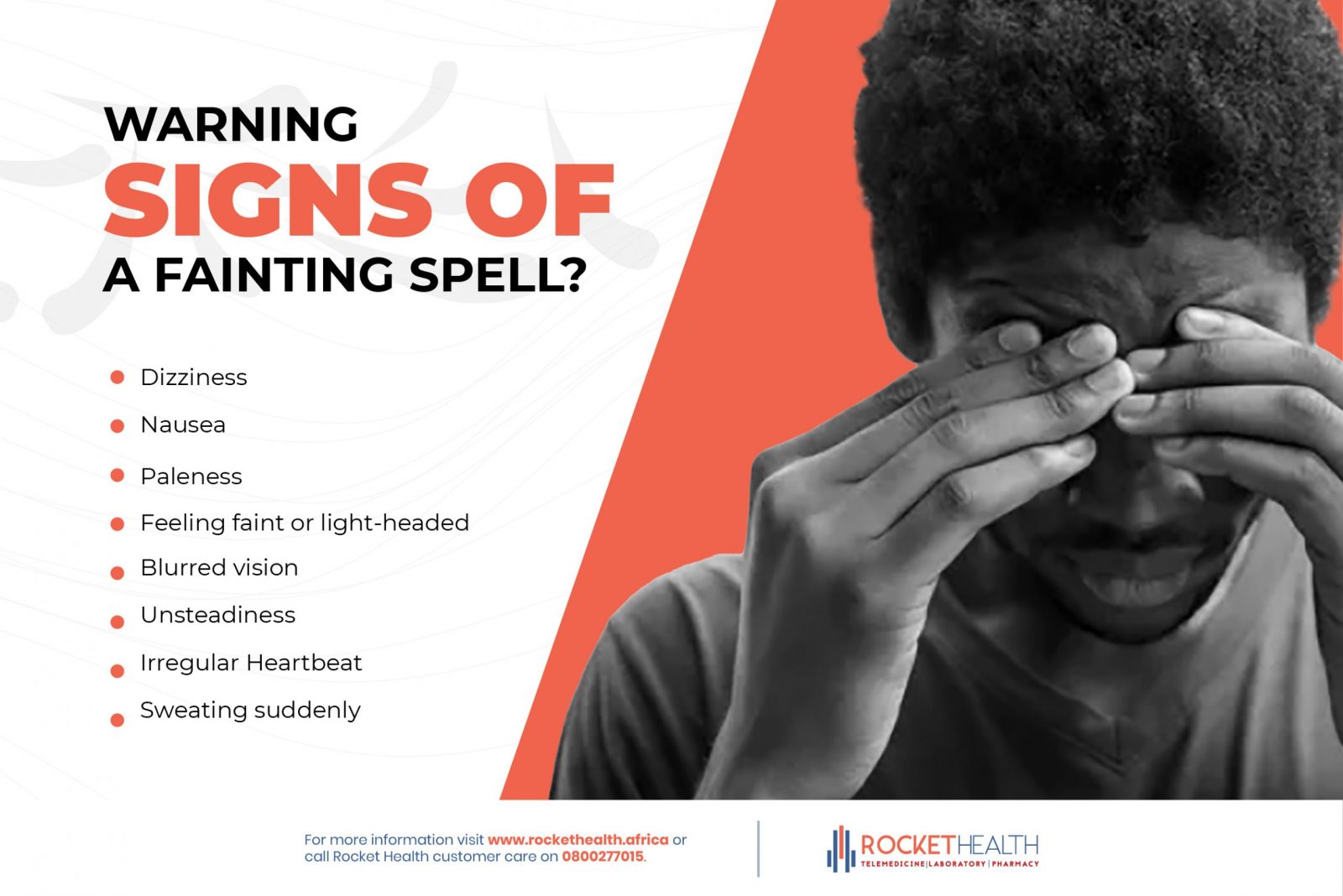
Symptoms of Fainting
The symptoms of fainting can vary depending on the underlying cause. However, common symptoms include:
- Dizziness or lightheadedness: This is often the first sign of an impending faint.
- Nausea or vomiting: These symptoms can occur before or after fainting.
- Weakness or fatigue: Feeling tired or weak can precede fainting.
- Blurred vision: Vision may become blurry or tunnel vision may occur.
- Cold sweats: The skin may become cold and clammy.
- Paleness: The skin may appear pale due to reduced blood flow.
- Rapid heartbeat: The heart may beat faster before fainting.
- Loss of consciousness: This is the hallmark of fainting.
Importance of Identifying the Cause of Fainting
Identifying the cause of fainting is crucial for determining the appropriate management strategy and preventing future episodes. While some causes of fainting are benign, others can indicate serious underlying medical conditions. Therefore, it is essential to seek medical attention if you experience fainting.
Diagnosis of Fainting
Diagnosing the cause of fainting typically involves a comprehensive medical evaluation, which may include:
- Medical History: A detailed medical history, including any past episodes of fainting, medications, and family history of heart disease, is essential.
- Physical Examination: The doctor will perform a physical examination to assess your overall health and look for any signs of underlying medical conditions.
- Electrocardiogram (ECG): This test records the electrical activity of the heart and can help identify arrhythmias.
- Holter Monitor: This portable device records the heart’s electrical activity over a 24-hour period, allowing for the detection of intermittent arrhythmias.
- Tilt Table Test: This test involves gradually tilting the patient upright on a table to simulate standing, monitoring blood pressure and heart rate to assess for orthostatic hypotension.
- Echocardiogram: This ultrasound imaging test assesses the structure and function of the heart.
- Blood Tests: Blood tests can help rule out underlying medical conditions, such as anemia or infection.
Management of Fainting
The management of fainting depends on the underlying cause. Treatment options may include:
- Lifestyle Modifications: For vasovagal syncope, simple lifestyle changes, such as staying hydrated, avoiding prolonged standing, and managing stress, can be helpful.
- Medications: Depending on the cause, medications may be prescribed to manage blood pressure, heart rate, or other underlying conditions.
- Pacemaker: For certain types of arrhythmias, a pacemaker may be implanted to regulate the heart rate.
- Surgery: In some cases, surgery may be necessary to correct underlying heart conditions.
FAQs about Fainting
Q: Is fainting dangerous?
A: While fainting can be alarming, it is often harmless and resolves on its own. However, fainting can be dangerous if it occurs while driving, swimming, or performing other activities that could lead to injury.
Q: How long does fainting last?
A: Fainting typically lasts for a few seconds to a few minutes. However, some individuals may experience longer episodes.
Q: What should I do if someone faints?
A: If someone faints, follow these steps:
- Check for responsiveness: Gently shake the person’s shoulder and ask if they are okay.
- Position them on their side: This helps prevent choking if they vomit.
- Check for breathing: Look, listen, and feel for breathing.
- Call for help: Call emergency medical services if the person is unresponsive or not breathing.
- Monitor the person: Continue to monitor their breathing and pulse until help arrives.
Q: When should I see a doctor about fainting?
A: It is important to see a doctor if you experience fainting, especially if:
- It is your first episode.
- You experience fainting frequently.
- You faint during strenuous activity or exertion.
- You have other symptoms, such as chest pain or shortness of breath.
- You have a family history of heart disease.
Tips to Prevent Fainting
- Stay hydrated: Dehydration can contribute to fainting, so drink plenty of fluids throughout the day.
- Avoid prolonged standing: If you have to stand for long periods, take breaks to sit down or elevate your legs.
- Manage stress: Practice relaxation techniques, such as deep breathing or meditation, to help manage stress.
- Avoid triggers: Identify and avoid situations that trigger your fainting episodes.
- Wear supportive shoes: Wear comfortable, supportive shoes that provide good arch support.
- Take medications as prescribed: If you are taking medications for any underlying medical conditions, take them as prescribed by your doctor.
Conclusion
Fainting is a common phenomenon with a wide range of underlying causes. While most fainting episodes are benign and resolve on their own, it is essential to seek medical attention to determine the underlying cause. Understanding the different types of fainting, their symptoms, and management strategies can help individuals take appropriate steps to prevent future episodes and ensure their safety. By being informed and proactive, individuals can minimize the risk associated with fainting and live healthy, fulfilling lives.






Closure
Thus, we hope this article has provided valuable insights into Understanding Fainting: Causes, Symptoms, and Management. We thank you for taking the time to read this article. See you in our next article!
